To Buy Cipro Online Visit Our Pharmacy ↓
 Cipro Resistant Bacteria: What You Need to Know
Cipro Resistant Bacteria: What You Need to Know
Ciprofloxacin, commonly known as Cipro, belongs to a class of broad-spectrum antibiotics called fluoroquinolones. Since its introduction in the late 20th century, it has become a crucial weapon in the fight against a wide range of bacterial infections. Its potency lies in its mechanism of action, which involves the inhibition of bacterial DNA gyrase and topoisomerase IV, enzymes critical for DNA replication and cell division. This allows Cipro to not only treat common infections like urinary tract infections and respiratory tract infections but also more severe conditions such as infectious diarrhea, bone and joint infections, and certain types of infectious colitis.
This antibiotic has been celebrated for its effectiveness against gram-negative bacteria, including strains that other antibiotics struggle to overcome. Its oral and intravenous formulations offer flexibility in treatment, catering to both outpatient settings and serious hospital-managed infections. With its expansive reach and the ability to penetrate deep into tissues, Cipro has been the drug of choice for numerous bacterial threats, making it an integral part of modern medical regimens. However, the widespread use of Cipro has also contributed to the gradual emergence of resistant bacteria, posing new challenges in the domain of infectious diseases.
The Rise of Cipro-resistant Strains
Ciprofloxacin, widely known as Cipro, has long been considered a potent antibiotic, commonly used to combat various bacterial infections. However, its widespread use has inadvertently contributed to the emergence of Cipro-resistant bacteria. These resistant strains are a growing concern in the medical community. They are resulting from genetic mutations and the acquisition of resistance genes, which enable them to survive even in the presence of the antibiotic. This phenomenon is not limited to any one region or country but is becoming a global issue, with resistant strains being reported in numerous countries and among various types of bacteria, notably including key pathogens such as Escherichia coli and particular strains of Staphylococcus aureus.
The development of resistance to Cipro is alarming as it jeopardizes treatment outcomes for patients suffering from serious infections. Instances of resistance have been recorded in both hospital and community settings, indicating a pervasive and widespread challenge. This trend mirrors the larger problem of antibiotic resistance, where once-reliable treatments become ineffective, leading to longer hospital stays, higher medical costs, and increased mortality rates. The growing ineffectiveness of Cipro highlights the need for vigilant use of antibiotics, improved detection methods for resistant strains, and accelerated research into alternative treatments and mitigation strategies.
Understanding How Bacteria Outsmart Antibiotics
Bacteria have evolved several strategies to survive in the face of antibiotic onslaughts. One common method is through the production of enzymes that neutralize the antibiotic's effects. In the case of Cipro, or ciprofloxacin, certain bacterial enzymes can modify the drug or break it down, rendering it ineffective. Another defense mechanism is the alteration of bacterial proteins that are the target sites for antibiotics. These slight structural changes can significantly reduce the antibiotic's ability to bind and inhibit the bacteria, thus allowing the bacteria to thrive even in the presence of the drug.
Additionally, bacteria can pump out antibiotics through membrane proteins, effectively decreasing the internal concentration of the drug below lethal levels. This is known as efflux, and the presence of efflux pumps can greatly contribute to the development of resistance. Another troubling aspect is the ability of bacteria to exchange genetic material, including genes responsible for antibiotic resistance. This horizontal gene transfer can happen through direct contact, the uptake of free DNA, or by bacterial viruses. Once a bacterium acquires resistance genes, it can replicate rapidly, spreading the resistance among its population and potentially transferring it to other bacterial species.
Health Implications of Antibiotic Resistance
Antibiotic resistance poses a formidable threat to public health, marking a pivotal challenge for modern medicine. The emergence of Cipro-resistant bacteria underscores a larger pattern of antimicrobial agents losing their efficacy against once-treatable infections. When bacteria become resistant, infections can persist, increasing the risk of spread and the potential for complications. This leads to prolonged hospital stays, the necessity for more aggressive and costly treatments, and, most critically, a higher mortality rate. Patients with compromised immune systems, such as those undergoing chemotherapy, are especially vulnerable, as their bodies are less equipped to fight off opportunistic infections.
The economic burden of antibiotic resistance also cannot be overstated. With fewer weapons in the arsenal against bacterial infections, the cost of healthcare escalates due to longer durations of care, additional laboratory tests to identify resistant strains, and the use of more expensive or less effective alternative treatments. Additionally, there is a reverberating impact on workplace productivity as individuals face extended illness and recovery periods. Such developments underscore the urgent need for new approaches in both the development of antimicrobials and the stewardship of existing treatments to safeguard their effectiveness for future generations.
Strategies to Combat Cipro Resistance
To effectively tackle the issue of ciprofloxacin resistance, healthcare providers and researchers emphasize the importance of judicious antibiotic use. This includes prescribing and utilizing ciprofloxacin only when it is unequivocally indicated, ensuring the correct dosage and duration are followed to minimize the selection pressure on bacteria. In clinical settings, antibiotic stewardship programs are instrumental, promoting the appropriate use of antimicrobials to preserve their effectiveness. Additionally, these programs provide education on the potential risks of overuse and misuse of antibiotics to healthcare professionals.
Alongside prudent antibiotic use, the development of novel therapeutics is crucial. Research is being directed toward discovering new antibiotics that can circumvent resistance mechanisms, as well as alternative therapies such as bacteriophages, vaccines, and probiotics that could reduce the reliance on traditional antibiotics. On a broader scale, public health initiatives focus on infection prevention through vaccination, improved sanitation, and the promotion of good hygiene practices. These strategies collectively aim to reduce the occurrence of infections, thereby decreasing the overall need for antibiotics and limiting the opportunity for the development of resistance.
Preventing the Spread of Resistant Bacteria
The containment of antibiotic resistance requires a multi-faceted approach involving the prudent use of antibiotics, adherence to infection control protocols, and public education. Healthcare providers play a crucial role by prescribing antibiotics only when necessary and ensuring the complete course is followed to prevent the survival of partially resistant bacteria. Patients are similarly responsible for taking antibiotics as directed and never sharing medication. In hospital settings, stringent infection control measures, including hand hygiene, using personal protective equipment, and regular disinfection routines, are essential to prevent the transmission of resistant strains.
In addition to medical practices, a broader perspective on antibiotic stewardship is needed. This includes monitoring and limiting the use of antibiotics in agriculture and the meat industry to reduce the environmental burden of antibiotics. Public health campaigns can enhance awareness about the dangers of overusing antibiotics and the importance of vaccination in reducing the need for antibiotics. Additionally, investments in research to develop new antibiotics and alternative treatments are vital for staying ahead in the arms race against evolving bacterial pathogens. Personal behaviors such as proper handwashing, avoiding close contact with sick individuals, and staying up to date with vaccinations can greatly reduce the risk of spreading resistant bacteria.
https://gaetzpharmacy.com/clomid.html https://buynoprescriptionrxxonline.net https://rxxbuynoprescriptiononline.com
Customer Service
Call us (702) 476-6762 or (858) 643-5555
Email address: awells@phamatech.com
PHAMATECH Las Vegas in the Media
COVID testing clinics report high volume of patients ahead of the new year
Angel Spears an operations coordinator for Phamatech said she expects more people to get tested after the new year’s eve weekend. “We’ve been quite busy, our system has been pretty efficient, fast in and out,” said Spears. Our turnaround time for our PCR test is 24 to 30 hours give or take and our rapid antigen is about 15 to 30 minutes.”
Las Vegas lab explains how it gets COVID-19 test results
"We went from about 40 to 70 people to ... 200 to 300 people a day," said Angela Spears, operations manager at Phamatech Labs in Las Vegas.
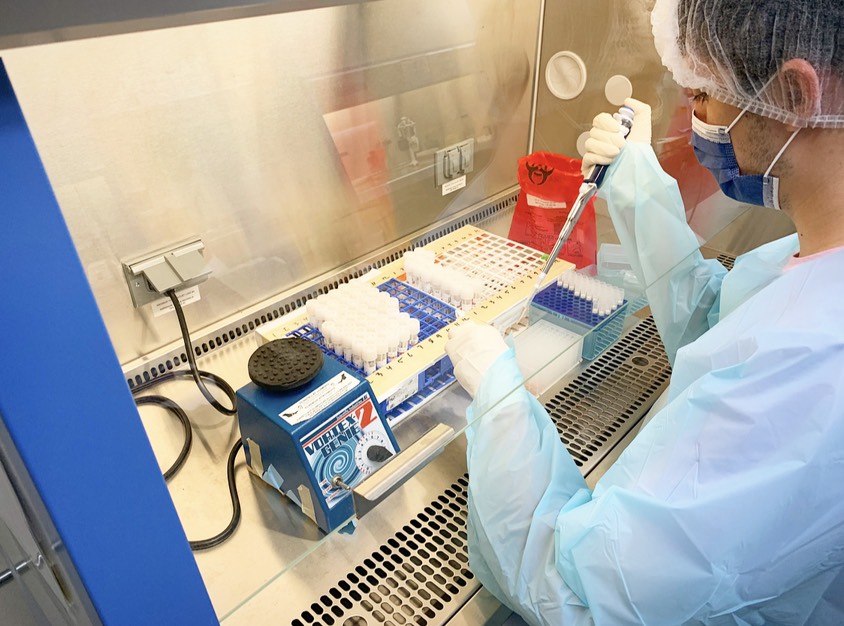
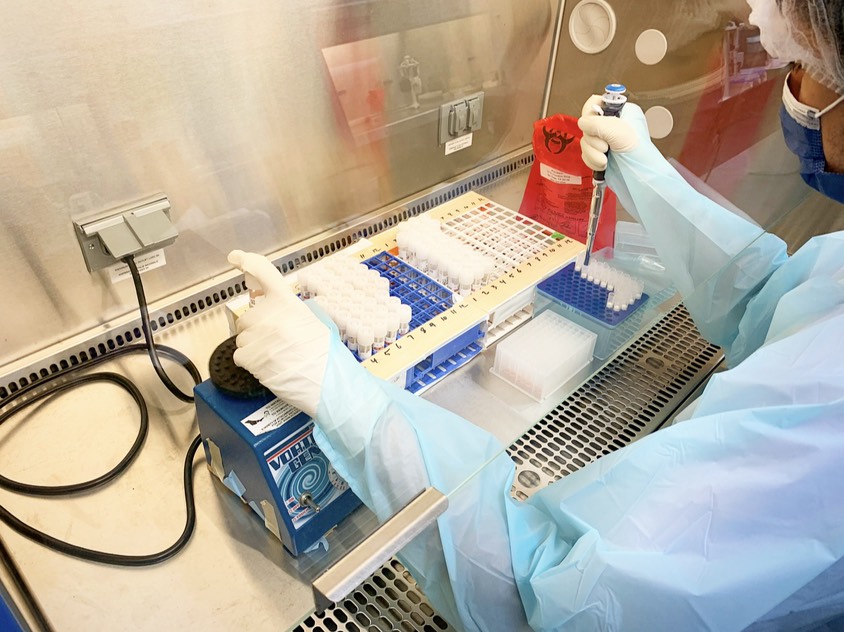
Our Laboratory


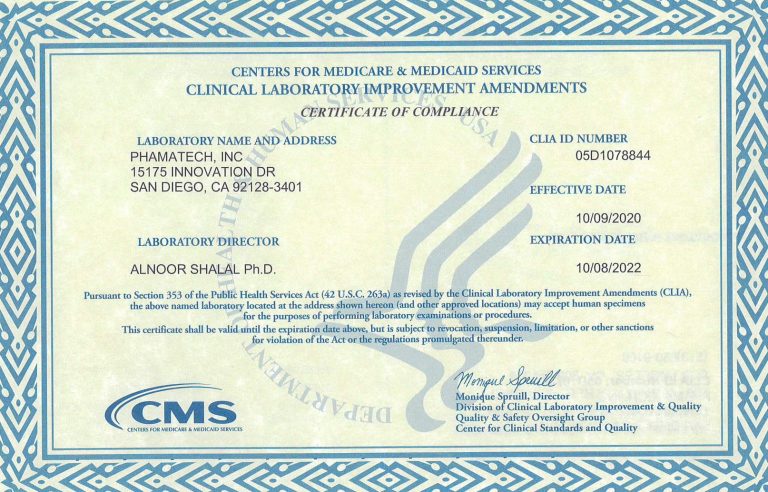
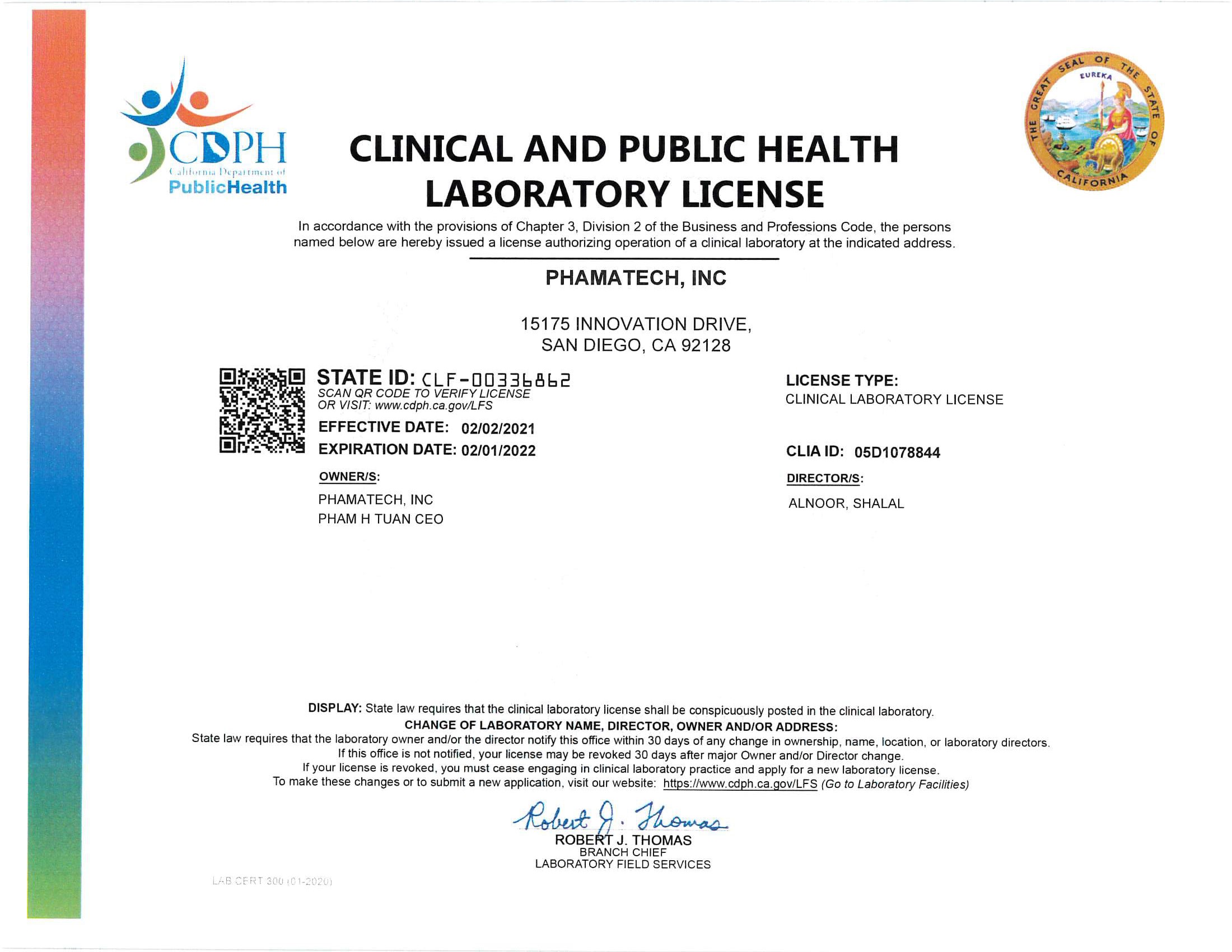
Laboratory Licenses and Certificates
.