To Buy Neurontin Online Visit Our Pharmacy ↓
 Debunking Myths: the Truth about Neurontin Side Effects
Debunking Myths: the Truth about Neurontin Side Effects
Neurontin, known generically as gabapentin, is a medication primarily used to manage seizures in epilepsy and to relieve neuropathic pain—pain caused by damage or dysfunction in the nervous system. Its role in the modulation of the nervous system is achieved through its action on the alpha-2-delta subunit of voltage-gated calcium channels in the brain, which reduces the release of excitatory neurotransmitters and stabilizes neural activity.
Though often associated with off-label use, such as for treating anxiety disorders, restless legs syndrome (RLS), and hot flashes, it is important to understand that Neurontin's approved indications are based on rigorous clinical testing. The drug is also commonly used in the management of postherpetic neuralgia, the lingering pain following an outbreak of shingles, reinforcing its significance in pain management medicine. With a clear grasp of Neurontin’s therapeutic intentions, patients and healthcare providers can better navigate its use and discuss legitimate expectations from its administration.
Common Misconceptions Vs. Documented Side Effects
Neurontin, known generically as gabapentin, is often entangled in a web of misinformation when it comes to its side effects. One prevailing myth suggests that the medication leads to rapid weight gain, an effect that isn’t substantiated by robust clinical evidence. In reality, while weight fluctuation can occur, it is not a universal side effect and often relates to other factors. Additionally, there's a widespread belief that Neurontin causes severe cognitive decline, yet studies show that while some individuals may experience mild drowsiness or dizziness, significant cognitive impairment is not a standard outcome.
Contrasting these misconceptions, documented side effects of Neurontin are usually mild and may include fatigue, unsteadiness, or peripheral edema. The literature emphasizes that serious side effects, such as severe allergic reactions or mood changes, are relatively rare. It’s crucial for users to understand that while any medication carries the risk of side effects, the likelihood and severity vary greatly among individuals. Patient education and open communication with healthcare providers are key in ensuring that the usage of Neurontin is managed eff
The Myth of Universal Experience with Neurontin
One of the pervasive myths surrounding Neurontin (gabapentin) is that it affects all individuals in the same way. This belief stems from a general misunderstanding of how drugs interact with the complex biology of the human body. In reality, the experience with Neurontin is subject to a wide range of factors including dosage, individual physiology, concurrent medications, and underlying health conditions. Not every patient will encounter the same side effects, and for many, the medication can be well-tolerated when used as prescribed.
To assume a uniform effect from Neurontin overlooks the variability of patient responses, a cornerstone principle in pharmacology. Researchers and clinicians have long recognized the role of genetic makeup, lifestyle, and even diet in influencing the efficacy and side effects of medications. The body’s reaction to Neurontin is no exception, with some patients reporting minimal issues while others may experience more pronounced side effects. This individual variability necessitates personalized medical guidance rather than reliance on anecdotal evidence or sweeping generalizations.
Investigating the Overstated Fear of Dependence
Neurontin, also known by its generic name gabapentin, was originally developed for the treatment of epilepsy but has since been widely prescribed for neuropathic pain and a variety of other neurological conditions. Public perception suggests a high potential for addiction and dependence, akin to that of opioids or benzodiazepines. However, clinical studies indicate that gabapentin does not fit the classic profile of addictive medications and has a lower potential for abuse. While any medication carries the risk of side-effect profiles that can lead to misuse, Neurontin's pharmacology does not typically lead to the dopaminergic reward pathways that are characteristic of addictive substances.
Nonetheless, reports of gabapentin misuse have surfaced, leading to heightened scrutiny and sometimes overstated fears regarding its potential for dependence. It is important to differentiate between physiological dependence, characterized by withdrawal symptoms upon cessation, and psychological dependence, where a patient may feel unable to function without the medication. The available evidence suggests that while withdrawal can occur, particularly with abrupt discontinuation after prolonged high-dose therapy, gabapentin dependence is generally not observed when the medication is used as prescribed. This distinction is crucial to both healthcare providers and patients to ensure Neurontin is used safely and effectively while mitigating unfounded concerns.
Neurontin in the Media: Separating Fact from Fiction
Media coverage of prescription medications like Neurontin (gabapentin) can often give rise to a blend of fact and myth, potentially leading to public misperceptions. Stories may highlight extreme cases or focus on off-label usage without providing the necessary context, which can distort the medication's risk profile. These narratives tend to cherry-pick data, omits mentioning the rigorous clinical trials that inform FDA approvals and the ongoing monitoring for adverse effects. It is crucial for consumers to critically evaluate these stories and seek information from reliable medical sources to understand the true nature of any medication.
Furthermore, anecdotal evidence presented in news segments or articles can contribute to a skewed understanding of Neurontin's side effects. Sensational reporting on legal cases involving the drug, or anecdotes from a subset of individuals who experienced adverse reactions, can amplify fears disproportionate to the actual risks for most patients. As such, it remains essential to contrast the reports in the media with peer-reviewed research and comprehensive data, ensuring a balanced view that recognizes both the benefits and the potential side effects of Neurontin as part of an informed health care decision-making process.
Beyond the Hype: Real Patients, Real Stories
When discussing the effects of medication like Neurontin, individual experiences add a valuable layer of insight that clinical data alone cannot provide. Personal testimonials reveal a spectrum of outcomes, ranging from those who have found relief without significant side effects to others who have encountered challenges in their treatment regime. For example, some epilepsy and neuropathic pain sufferers share success stories of regained functionality and improved quality of life, emphasizing the medication’s positive impact when other treatments had failed.
Conversely, a subset of patients reports experiences that resonate less with medical studies and more with the less common or under-discussed side effects. These narratives often highlight the complexities of managing side effects and the importance of personalized medical guidance. They serve as crucial reminders that while statistical averages are informative, the variability between individuals necessitates a tailored approach to treatment. The real-world stories of Neurontin users underscore the necessity for open dialogue between patients and healthcare providers to navigate the course of therapy effectively.
http://metabolicleader.com/images/homepage_extras/png/symbicort-inhaler.html https://imed.isid.org/wp-content/languages/themes/po/aciphex.html https://www.soundviewmed.com/wp-content/uploads/2022/08/png/phenergan.html
Customer Service
Call us (702) 476-6762 or (858) 643-5555
Email address: awells@phamatech.com
PHAMATECH Las Vegas in the Media
COVID testing clinics report high volume of patients ahead of the new year
Angel Spears an operations coordinator for Phamatech said she expects more people to get tested after the new year’s eve weekend. “We’ve been quite busy, our system has been pretty efficient, fast in and out,” said Spears. Our turnaround time for our PCR test is 24 to 30 hours give or take and our rapid antigen is about 15 to 30 minutes.”
Las Vegas lab explains how it gets COVID-19 test results
"We went from about 40 to 70 people to ... 200 to 300 people a day," said Angela Spears, operations manager at Phamatech Labs in Las Vegas.
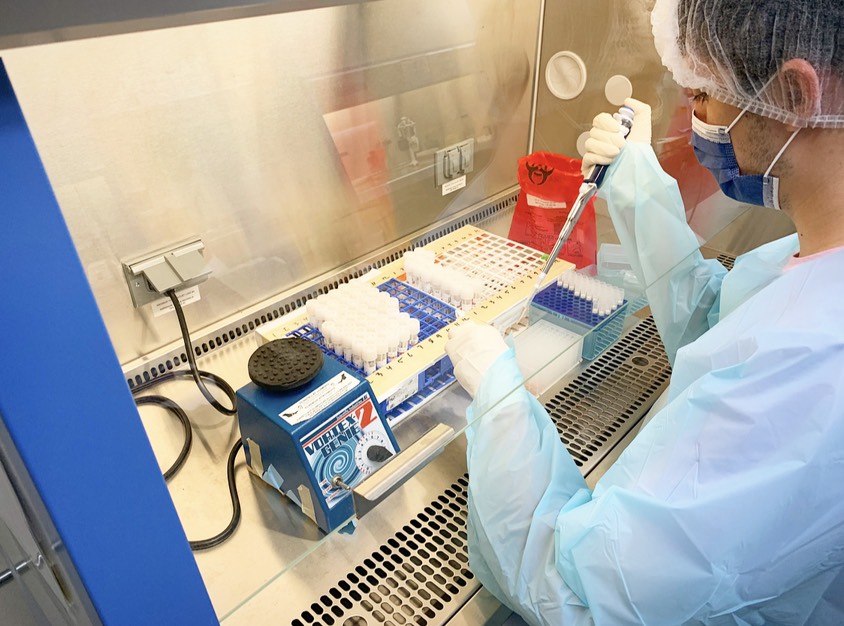
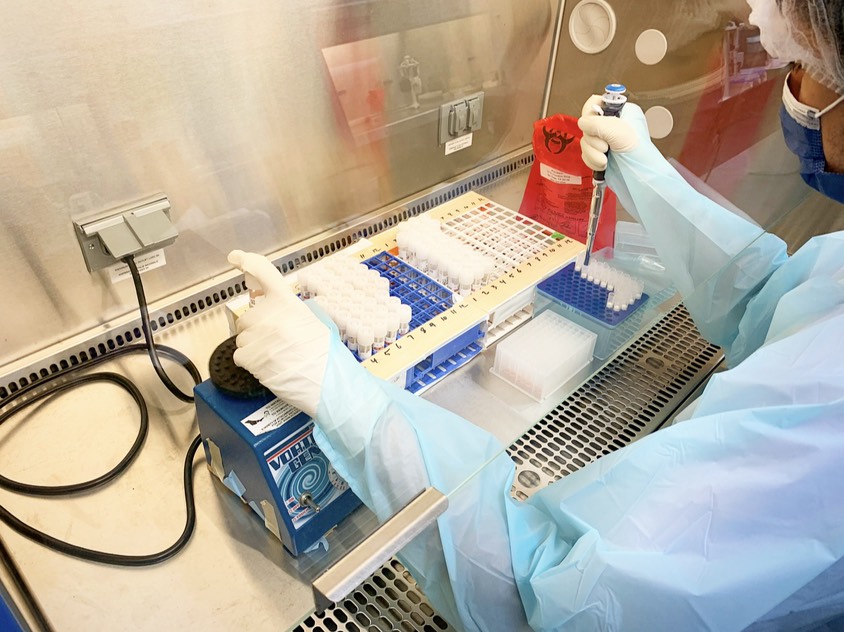
Our Laboratory


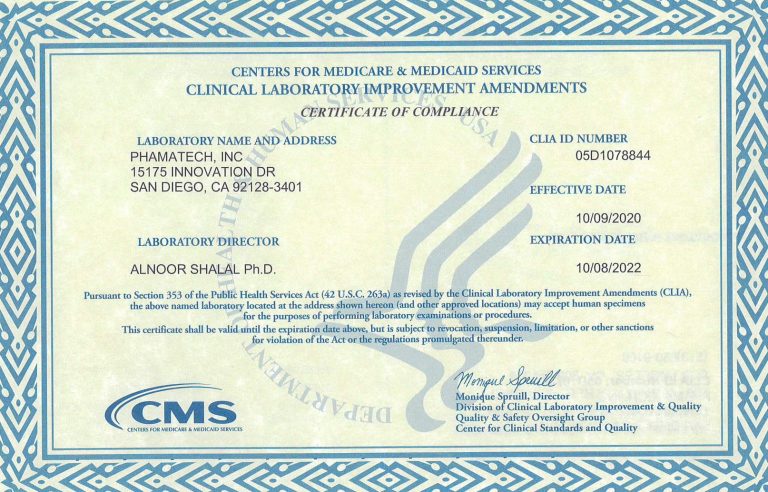
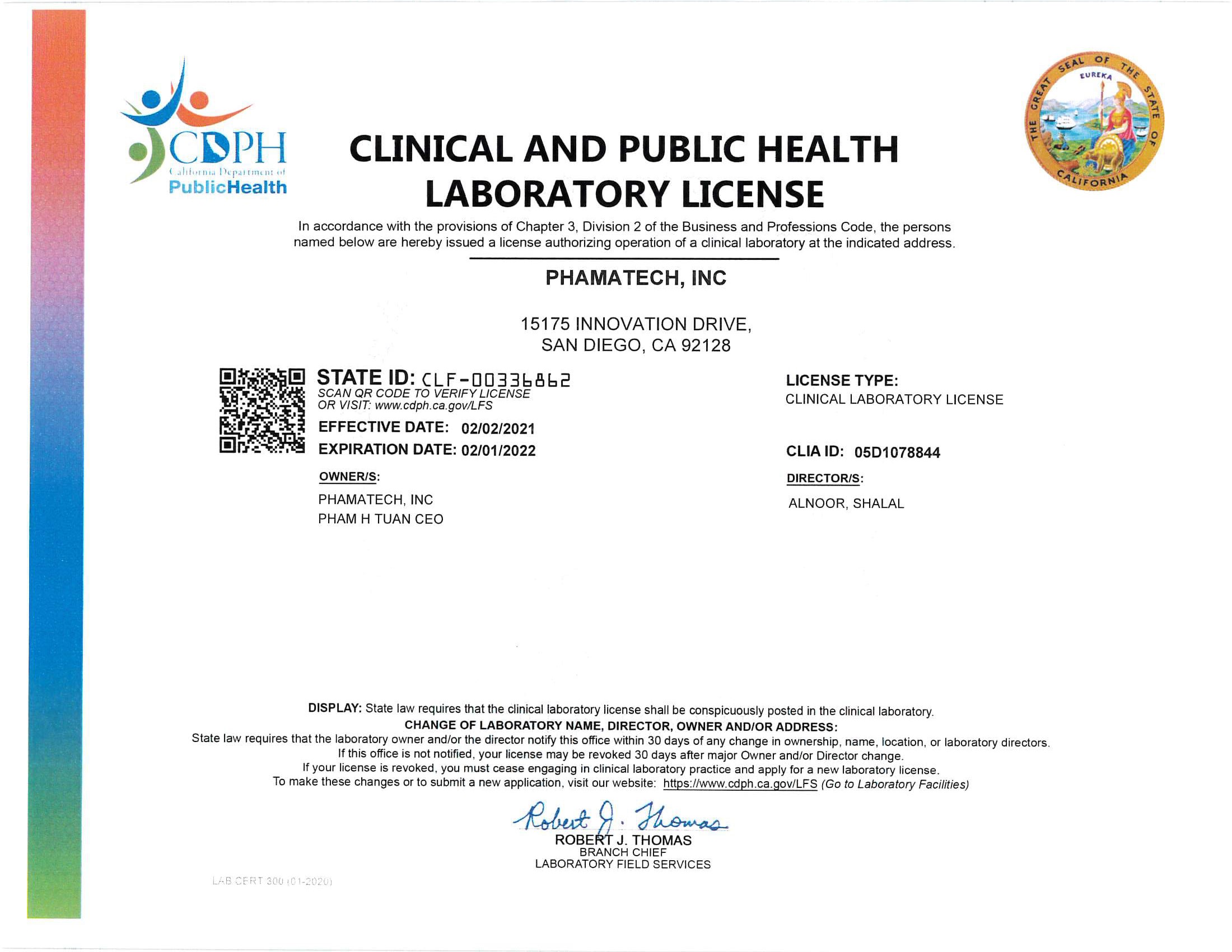
Laboratory Licenses and Certificates
.