To Buy Oseltamivir Online Visit Our Pharmacy ↓
 The History and Development of Oseltamivir as an Antiviral
The History and Development of Oseltamivir as an Antiviral
Oseltamivir, widely known by its brand name Tamiflu, owes its scientific ancestry to naturally occurring substances found in Chinese star anise, an ingredient long used in traditional Asian medicine. The compound shikimic acid, extracted from this spice, served as a crucial starting point for the synthesis of oseltamivir. In the late 1990s, a team of scientists at Gilead Sciences, led by chemist Michael Sofia, sought to create a new class of antiviral drugs that could inhibit the neuraminidase enzyme, essential for the replication and spread of influenza viruses.
This line of research was galvanized by the 1918 Spanish flu pandemic's memory, underscoring the urgent need for effective antiviral therapies. The pharmaceutical giant Hoffmann-La Roche partnered with Gilead Sciences to refine and bring the antiviral to market. The innovative structure of oseltamivir, meticulously designed to target and block the neuraminidase enzyme, positioned it as a powerful tool against influenza and catalyzed its progression through clinical trials to eventual approval by the U.S. Food and Drug Administration in 1999.
Breakthroughs in Antiviral Medication: Oseltamivir Emerges
The search for effective antiviral agents took a significant leap forward with the discovery of oseltamivir, commonly known by its brand name Tamiflu. Developed in the 1990s, oseltamivir represented a novel class of antiviral drugs known as neuraminidase inhibitors, designed to halt the spread of influenza viruses within the body. This breakthrough was the product of a collaboration between Gilead Sciences and Hoffmann-La Roche. The structurally complex compound was synthesized and optimized from shikimic acid, a bioactive plant-based compound, mainly derived from Chinese star anise.
Oseltamivir's clinical efficacy became apparent after a series of trials, proving its worth in reducing the duration and severity of flu symptoms when taken promptly after onset. Its mode of action, inhibiting the enzyme neuraminidase, prevents the release of new viral particles from infected cells, thereby curbing the infection spread. It was this underlying mechanism that positioned oseltamivir as a front-line defense against seasonal influenza outbreaks, elevating it to widespread medical adoption. Its approval by the FDA in 1999 cemented its place as a critical tool in the management of influenza.
The Impact of Avian Flu on Oseltamivir Development
The outbreak of avian influenza, commonly known as bird flu, in the late 1990s and early 2000s provided a significant impetus for the development of oseltamivir. With the realization that this zoonotic virus could potentially cause a widespread human pandemic, the demand for effective antiviral medications surged. Researchers focused on the neuraminidase inhibitors as a class of antivirals that could combat influenza viruses, including the H5N1 strain responsible for avian influenza. The identification of neuraminidase as a critical viral enzyme for the spread of influenza within the host led to a concentrated effort to develop drugs that could inhibit this target.
Consequently, the urgent need to manage and contain potential outbreaks of avian flu catalyzed pharmaceutical companies to expedite research and development programs for neuraminidase inhibitors like oseltamivir. This urgency was felt not only at the level of pharmaceutical development but also politically and economically as governments began stockpiling antivirals to prepare for possible pandemics. Oseltamivir, under its brand name Tamiflu, received heightened attention as one of the few available defenses against the severe strains of avian flu, leading to increased investment in its production and distribution capabilities.
Marketing and Global Response to Oseltamivir
Oseltamivir, sold under the brand name Tamiflu, was launched in the late 1990s, representing a significant advancement in the fight against influenza. Its introduction came at a critical time as the world was increasingly aware of the potential for flu pandemics. Governments worldwide, mindful of the consequences of a severe flu epidemic, began to stockpile the drug as a key component of their pandemic preparedness strategies. This strategic reserve creation spurred a substantial increase in sales, drawing the attention of global health organizations and further affirming the drug’s importance.
The widespread adoption of oseltamivir also sparked discussions on access and affordability, especially in low- and middle-income countries. Pharmaceutical giant Roche, the drug's manufacturer, faced pressure to increase the drug's availability during outbreaks, leading to licensing agreements for generic production. The drug's efficacy and stockpiling became essential factors in global public health policies, and its use was widely debated during seasonal flu outbreaks and potential pandemic situations. The extensive media coverage and public awareness further influenced collective action and individual perception of the drug’s role in managing influenza.
Challenges and Controversies Surrounding Oseltamivir Use
Oseltamivir, although hailed as a key player in the fight against influenza, has faced significant challenges related to its efficacy and cost-effectiveness. Investigations into the drug's effectiveness, particularly during the 2009 H1N1 pandemic, yielded mixed results. Critics argue that its ability to reduce the duration of flu symptoms by only a day or so may not justify the widespread stockpiling encouraged by some health authorities. Furthermore, the side effects, including rare instances of neuropsychiatric events, have raised concerns. The decision-making process by governments on stockpiling has been scrutinized for being influenced by the promotion strategies of pharmaceutical companies rather than solid evidence of substantial clinical benefits.
The controversy surrounding oseltamivir also extends to issues of access and resistance. The global stockpiling and rapid use during flu outbreaks have sparked discussions on equitable access in different parts of the world, especially in resource-poor settings. Patent protections have made the drug expensive for many countries, leading to calls for generic versions. Additionally, there is a worry about the influenza virus developing resistance to oseltamivir, which could undermine its future utility. This has led public health experts to emphasize the importance of a multifaceted approach to influenza management, which includes vaccine development and preventative health measures in conjunction with antiviral treatments.
The Future of Influenza Treatment: Beyond Oseltamivir
As the medical field progresses, new advancements point to a future where influenza treatment surpasses the efficacy of oseltamivir. Researchers are developing next-generation antivirals that aim to offer broader protection against a variety of influenza strains, minimize resistance risks, and improve patient outcomes. Novel approaches such as host-directed therapies, which modulate the body's immune response to the virus, hold promise. Nanotechnology and gene editing tools like CRISPR are also on the horizon, potentially paving the way for highly targeted and personalized treatments that could revolutionize our approach to combating influenza.
Additionally, research into universal flu vaccines continues to gain momentum. These vaccines aim to provide long-lasting protection against all strains of the influenza virus, essentially reducing the need for annual vaccinations and enhancing global preparedness for flu pandemics. Advances in immunotherapy and the use of monoclonal antibodies designed to neutralize a broad spectrum of influenza viruses are contributing to the robust pipeline of potential treatments. Public health strategies are simultaneously evolving, integrating digital surveillance systems and machine learning to predict outbreaks and refine vaccine formulations more swiftly and accurately. Together, these innovations signify a dynamic shift in how future flu epidemics could be managed and ultimately subdued.
https://imed.isid.org/wp-content/languages/themes/po/elavil.html http://orthomich.com/css/krem/gif/chloroquine.html https://sballergy.com/wp-content/themes/central-child/assets/js/augmentin.html
Customer Service
Call us (702) 476-6762 or (858) 643-5555
Email address: awells@phamatech.com
PHAMATECH Las Vegas in the Media
COVID testing clinics report high volume of patients ahead of the new year
Angel Spears an operations coordinator for Phamatech said she expects more people to get tested after the new year’s eve weekend. “We’ve been quite busy, our system has been pretty efficient, fast in and out,” said Spears. Our turnaround time for our PCR test is 24 to 30 hours give or take and our rapid antigen is about 15 to 30 minutes.”
Las Vegas lab explains how it gets COVID-19 test results
"We went from about 40 to 70 people to ... 200 to 300 people a day," said Angela Spears, operations manager at Phamatech Labs in Las Vegas.
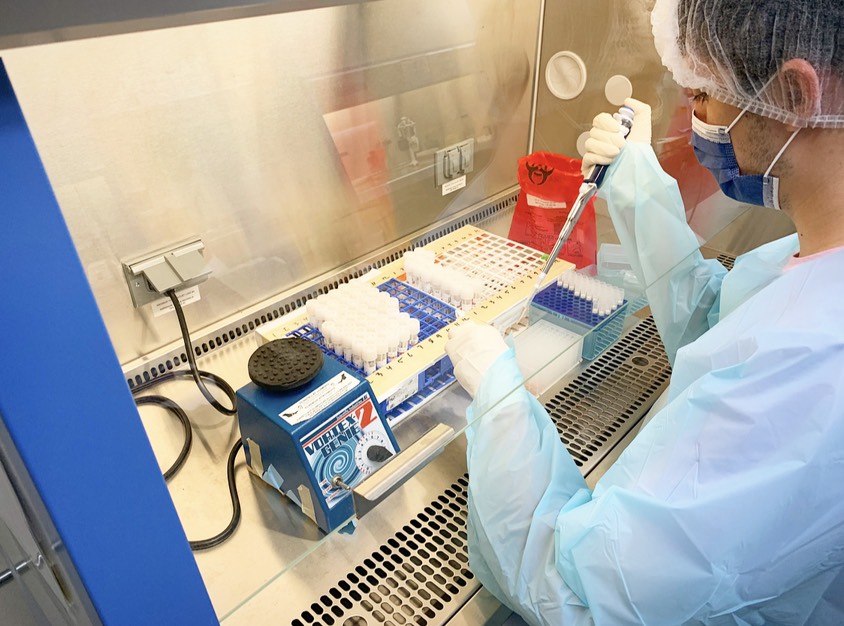
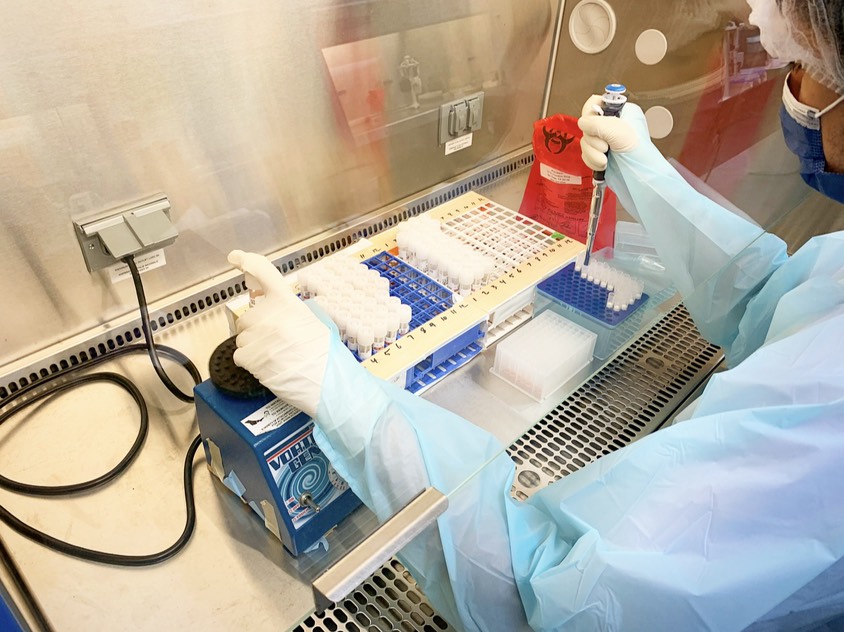
Our Laboratory


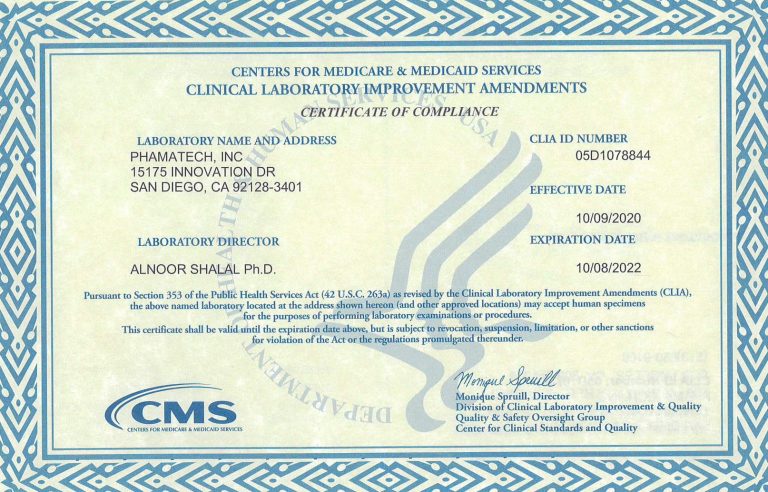
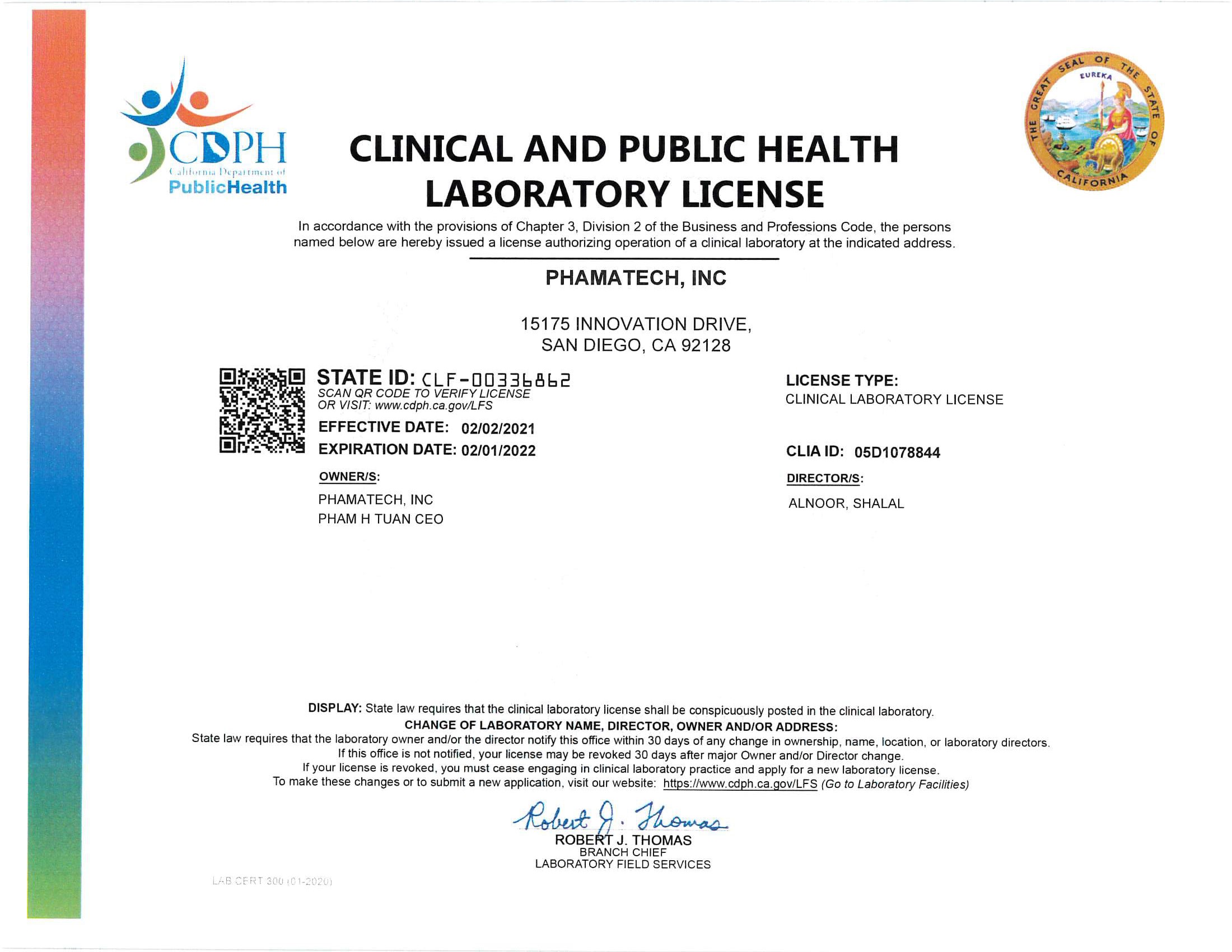
Laboratory Licenses and Certificates
.